Differences in Chronic Pain for Men and Women
Doctors and scientists have not traditionally distinguished pain treatment in men and women. Typically, they are treated with similar drugs and protocols.
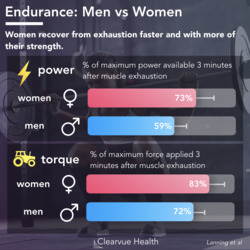
However, new research is increasingly showing significant differences in the way men and and women experience pain.
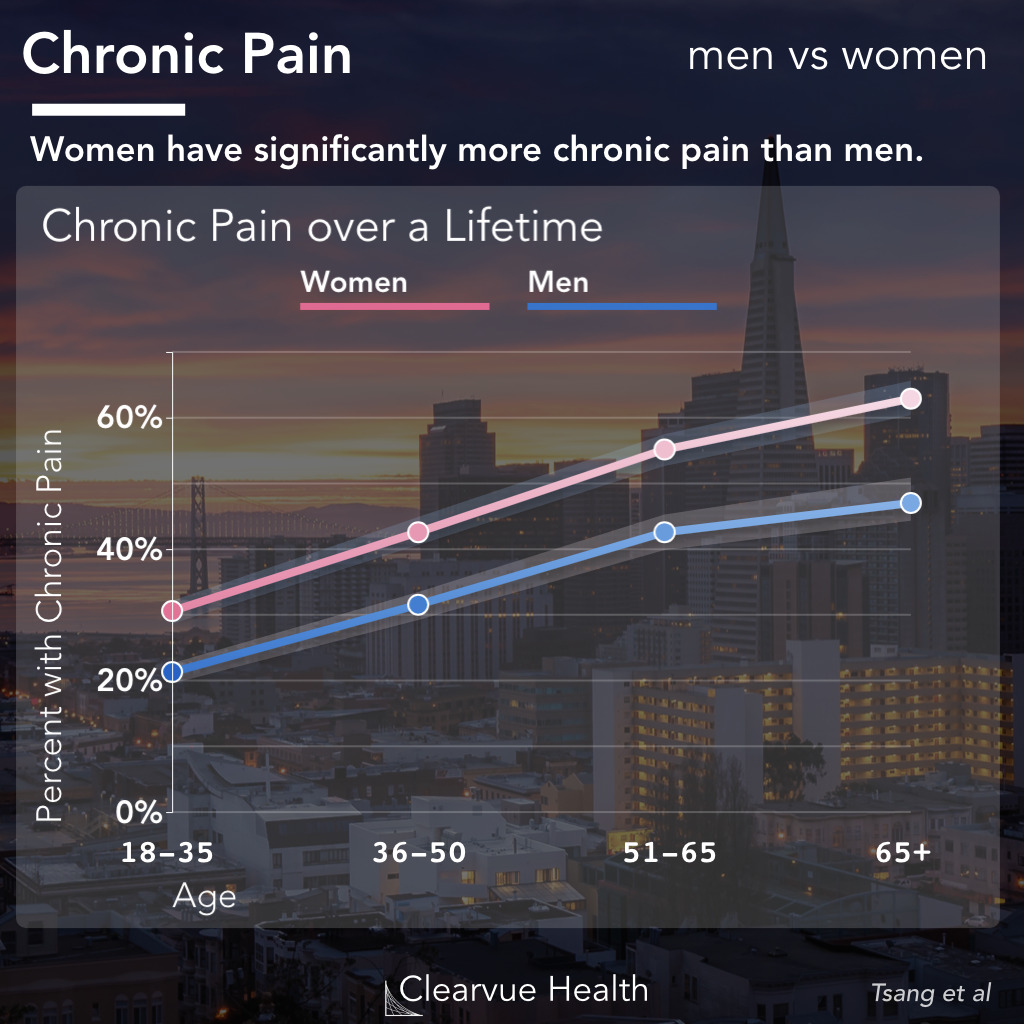
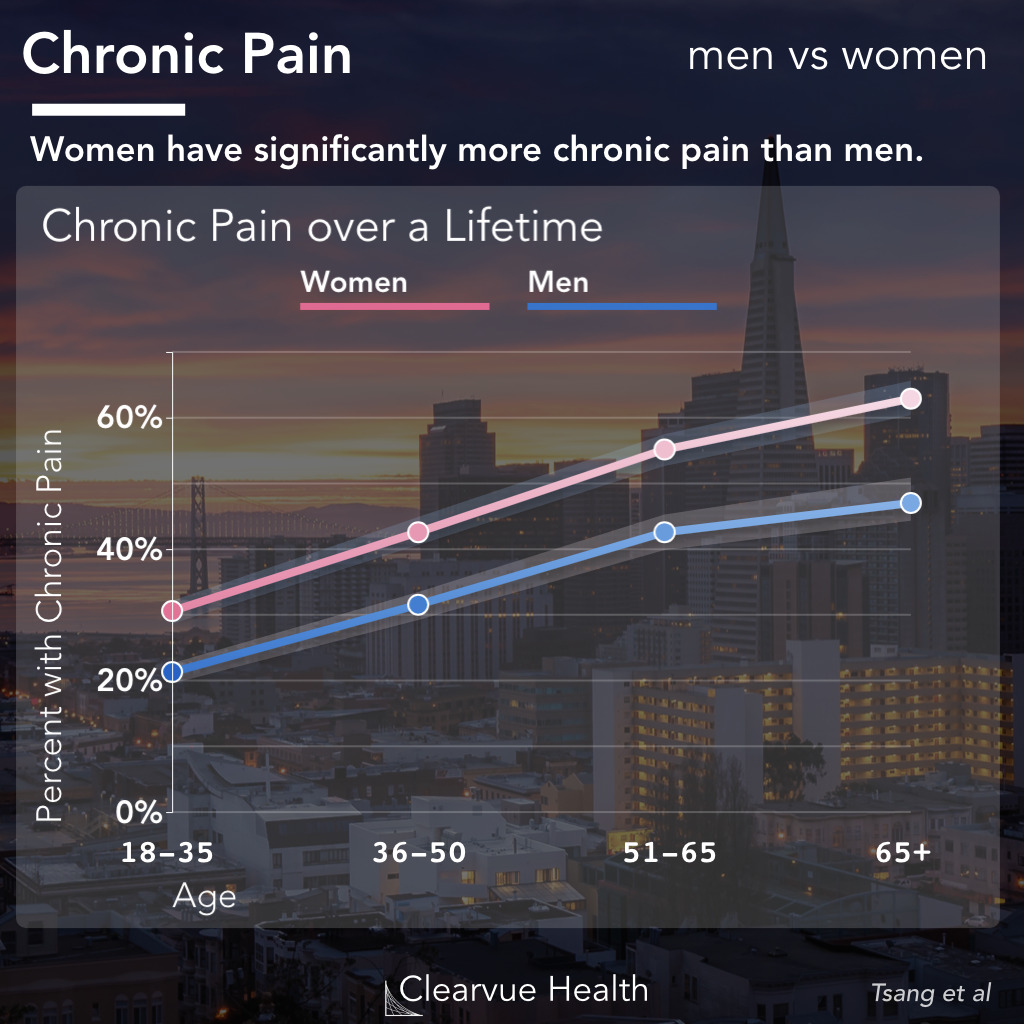
An international research effort looked at chronic pain across 17 countries to provide one of the most comprehensive snapshots of pain across gender and age.
They found that all other factors being equal, a women is significantly more likely to experience chronic pain than men.
This pattern appears consistently across many countries, both developed and developing.
As the authors write:
“
Despite wide variation in socioeconomic, demographic, and cultural characteristics across the participating countries, and in the country-specific prevalence rates of chronic pain conditions, several findings were cross-nationally consistent. Females exhibited a higher overall prevalence of chronic pain than males, a finding in line with prior research.
Source: Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders.
Gender Transition and Chron ic Pain
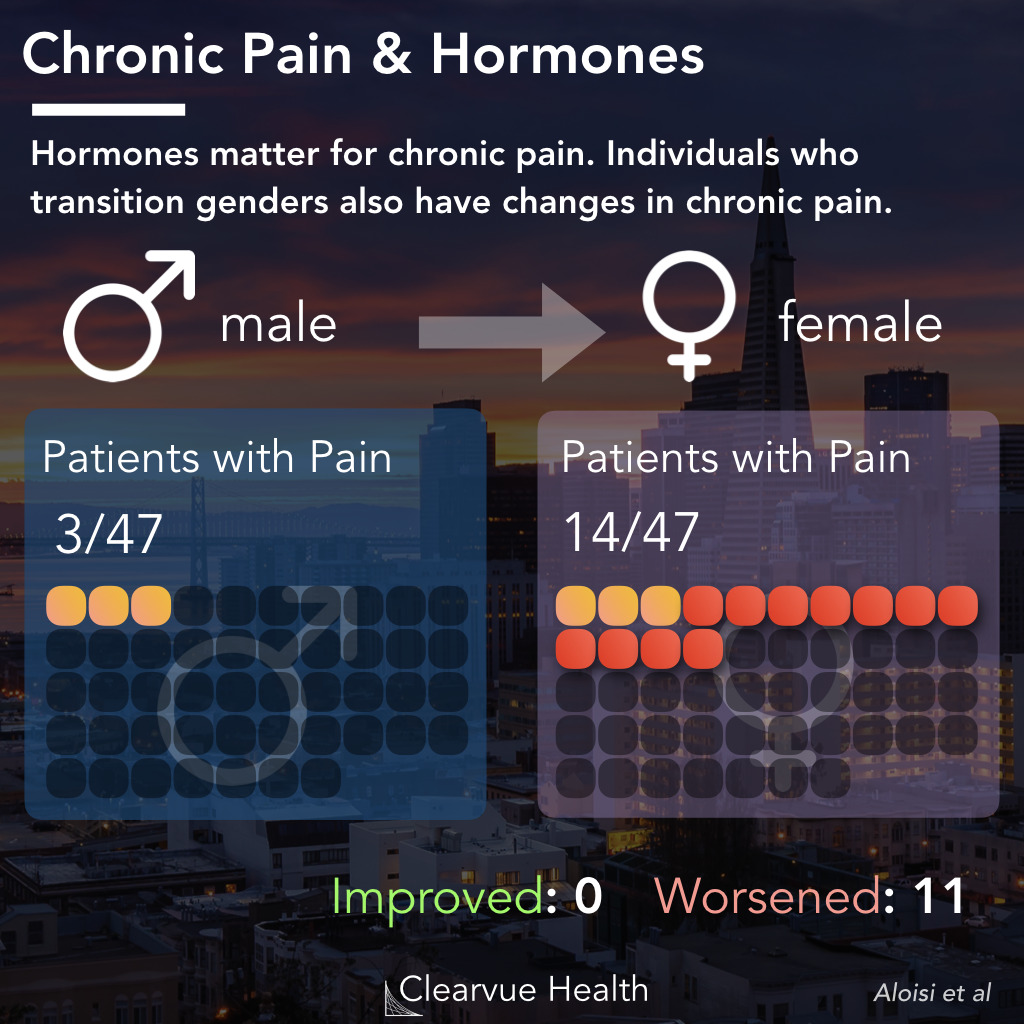
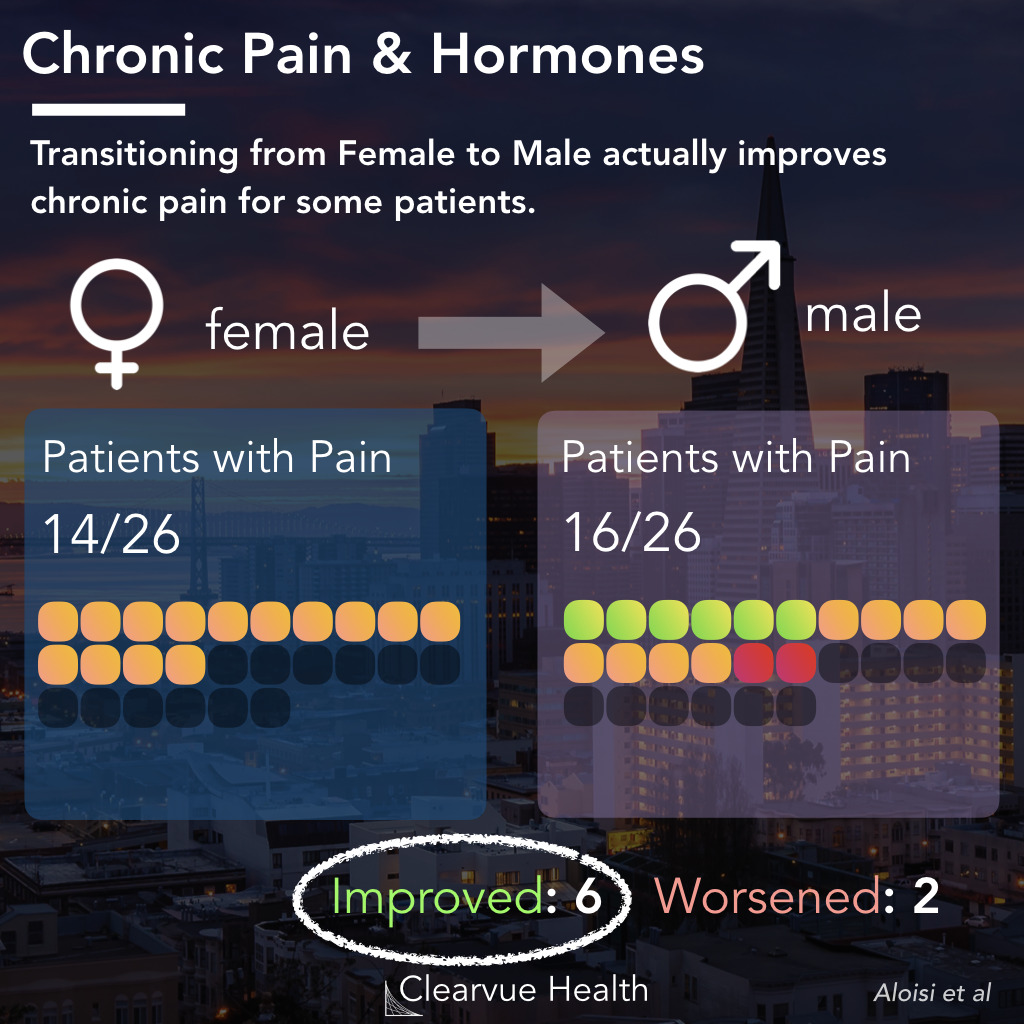
A study on individuals who transition genders shows that the relationship between gender and pain may be at least in part biological and driven by hormones.
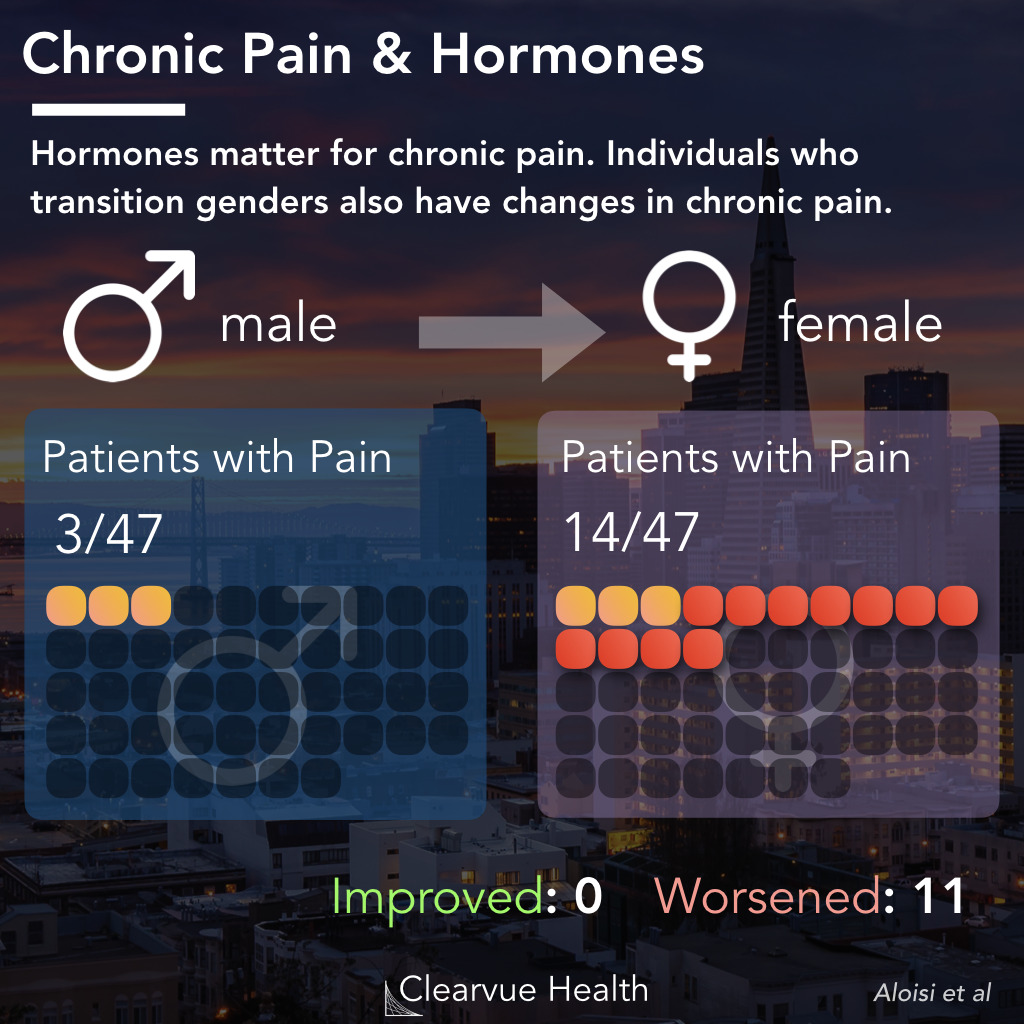
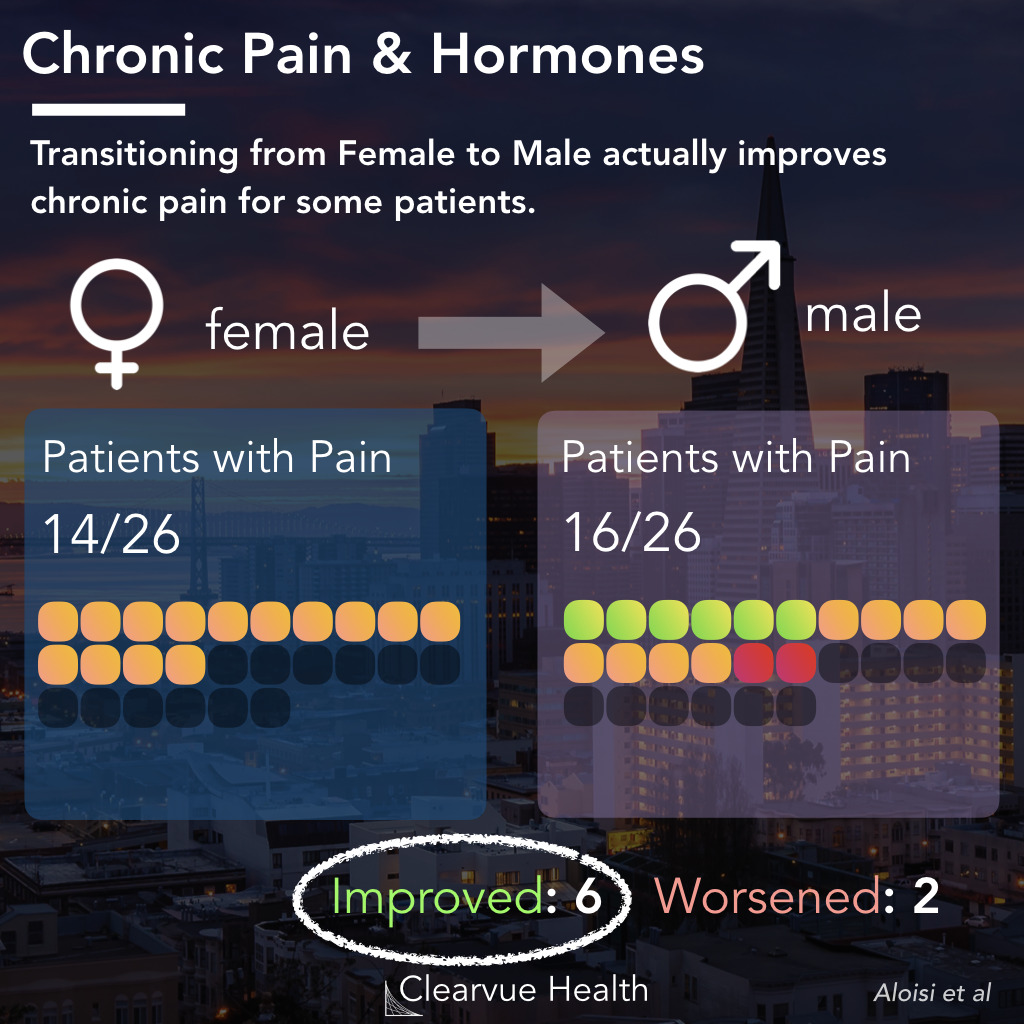
In a study of transgendered volunteers before and after their gender transition, researchers found that hormone therapy’s effect on chronic pain may depend on the type of transition.
Transitioning from Male to Female caused 11/47 patients studied to develop chronic pain, which is a substantial number in a relatively short amount of time.
However, transitioning the opposite direction, from female to male, actually helped some patients with their pain. Out of the 26 female to male volunteers in the study, 11 reported improvement in their pain. Only 2 developed pains that were not present before the study.
It is certainly plausible that the transitioning process adds stresses to the mind and body. However, the fact that this additional pain mostly occurred only in one direction suggests that at least some of the differences in pain between men and women may be driven by hormones. As the authors themselves wrote:
“
These findings support experimental data in animals and clinical data in humans suggesting that sex steroid hormones play an important role in pain.
Source: Cross-sex hormone administration changes pain in transsexual women and men
Data on Gender Differences in Pain in Mice
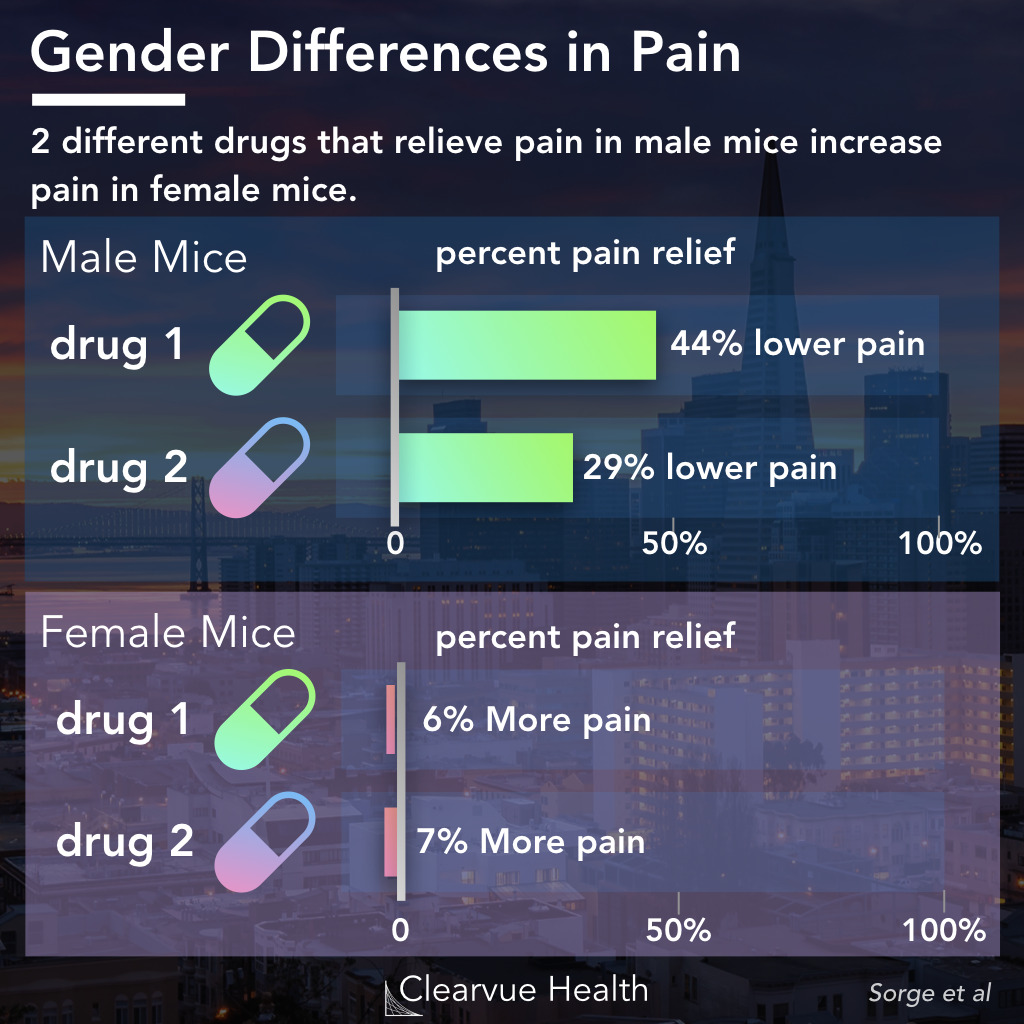
Studies on the biology of pain in mice show that there may be additional neurological differences between men and women that we don’t yet know about.
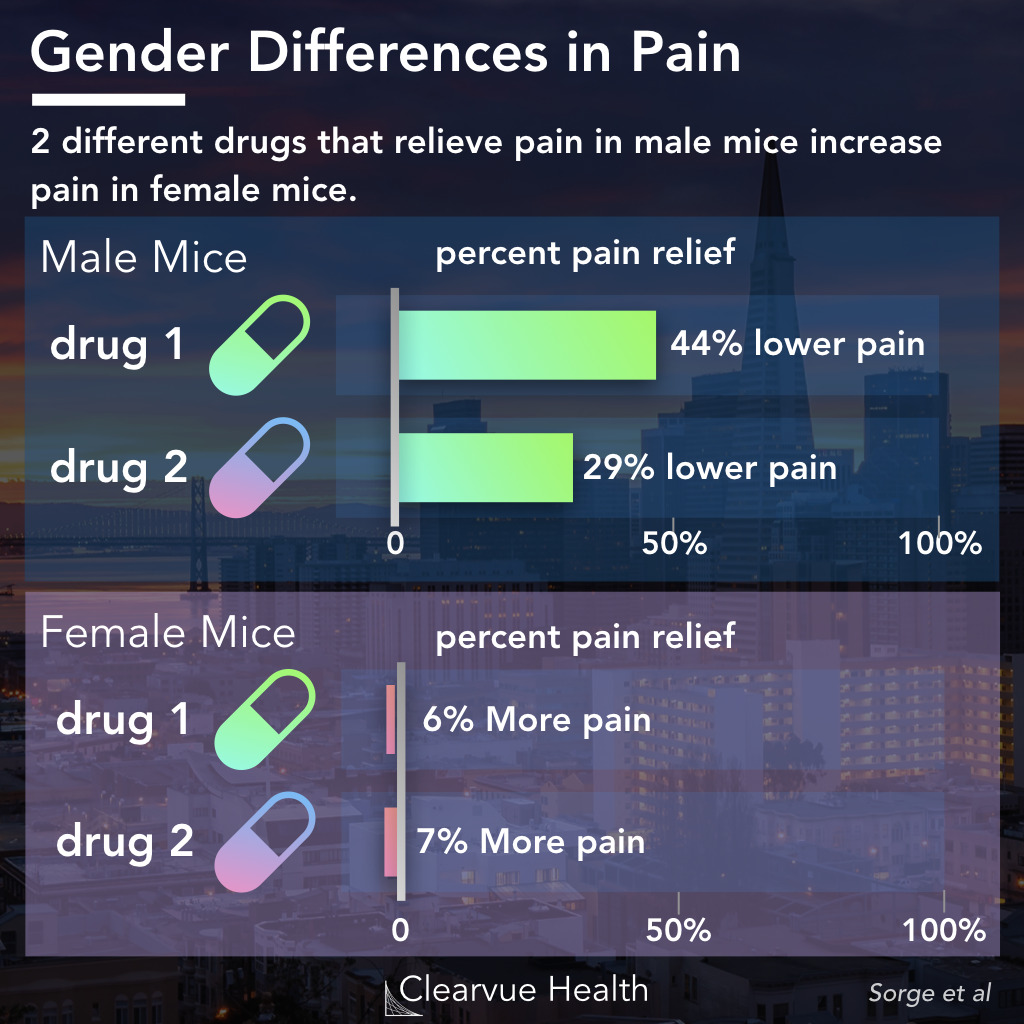
In an experiment testing different experimental pain relievers in male and female mice, researchers found that several compounds only relieved pain in male mice. While they relieved around 50% of the pain in male mice, they actually increased pain in some female mice.
This demonstrated that some pain pathways, which we are still working to understand, have fundamentally different mechanisms in male and female mice. This has not been replicated in humans yet, but there is a good chance at least some of this effect may be present in humans as well.
Source: Different immune cells mediate mechanical pain hypersensitivity in male and female mice.
Why This Matters
Many in the healthcare profession have been dismissive of chronic pain, particularly in female patients.
Part of this may be because we don’t have good therapies for the pain, part of this may be culture passed down through generations of doctors, part of this may be sexism.
In any case, the finding that biology drives gender differences in chronic pain provides further strong evidence that chronic pain in women should be taken seriously as a medical issue. It’s real, it’s biological, and it’s a significant burden for many.
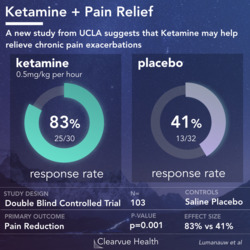
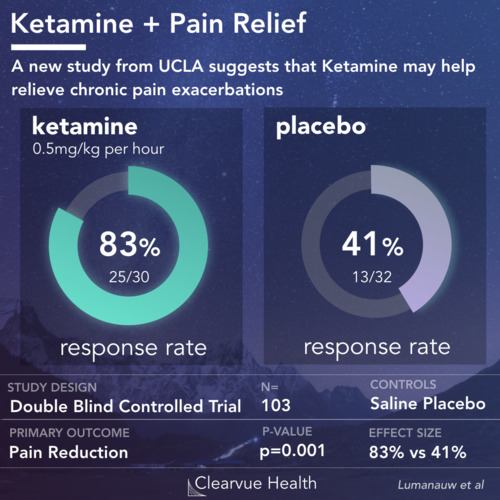
Chronic pain remains one of the most significant unmet medical needs. Millions around the world live in chronic or constant pain with no good solutions.
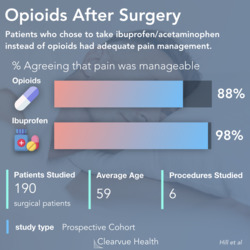
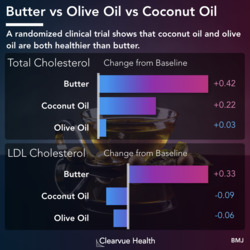
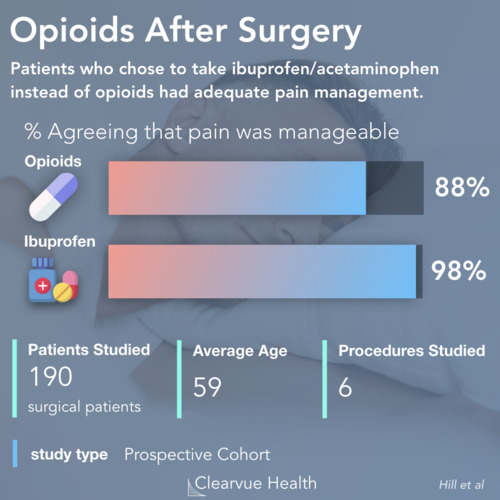
Opioid painkillers are our best treatment against pain. However, they carry significant addiction risks. They also become less effective over time with chronic use.
As we get better at treating pain, and as new therapies come down the pipeline, it may be time to consider developing and testing drugs with these gender differences in mind.
As the authors of one of the first studies to coin the term “Gender Pain Gap” wrote:
“
There’s a real possibility that pain drugs that failed clinical trials in the past might have succeeded if they had been tested separately by sex
Amber Dance
Source: Why the sexes don’t feel pain the same way