Diabetes and Mental Health: Are people with diabetes at higher risk for psychiatric disorders?
Diabetes is a chronic health condition that affects how your body turns food into energy. Type 1 diabetes is thought to be caused by an autoimmune reaction most commonly in childhood. Type 2 diabetes typically develops in adulthood when the body can not maintain healthy blood sugar levels. There is currently no way to prevent type 1 diabetes. Type 2 diabetes can be prevented with healthy lifestyle changes but some people are at higher risk than others.
Source: CDC What is Diabetes?
Being a chronic condition, diabetes does not go away. Most diabetes patients must take insulin every day to survive. As you can imagine, managing diabetes can take a significant toll on a patient. Those with diabetes need to regularly check their blood sugar, monitor their diet, and speak with their physicians. The constant demands of diabetes can have an impact on a patient's mental well-being.
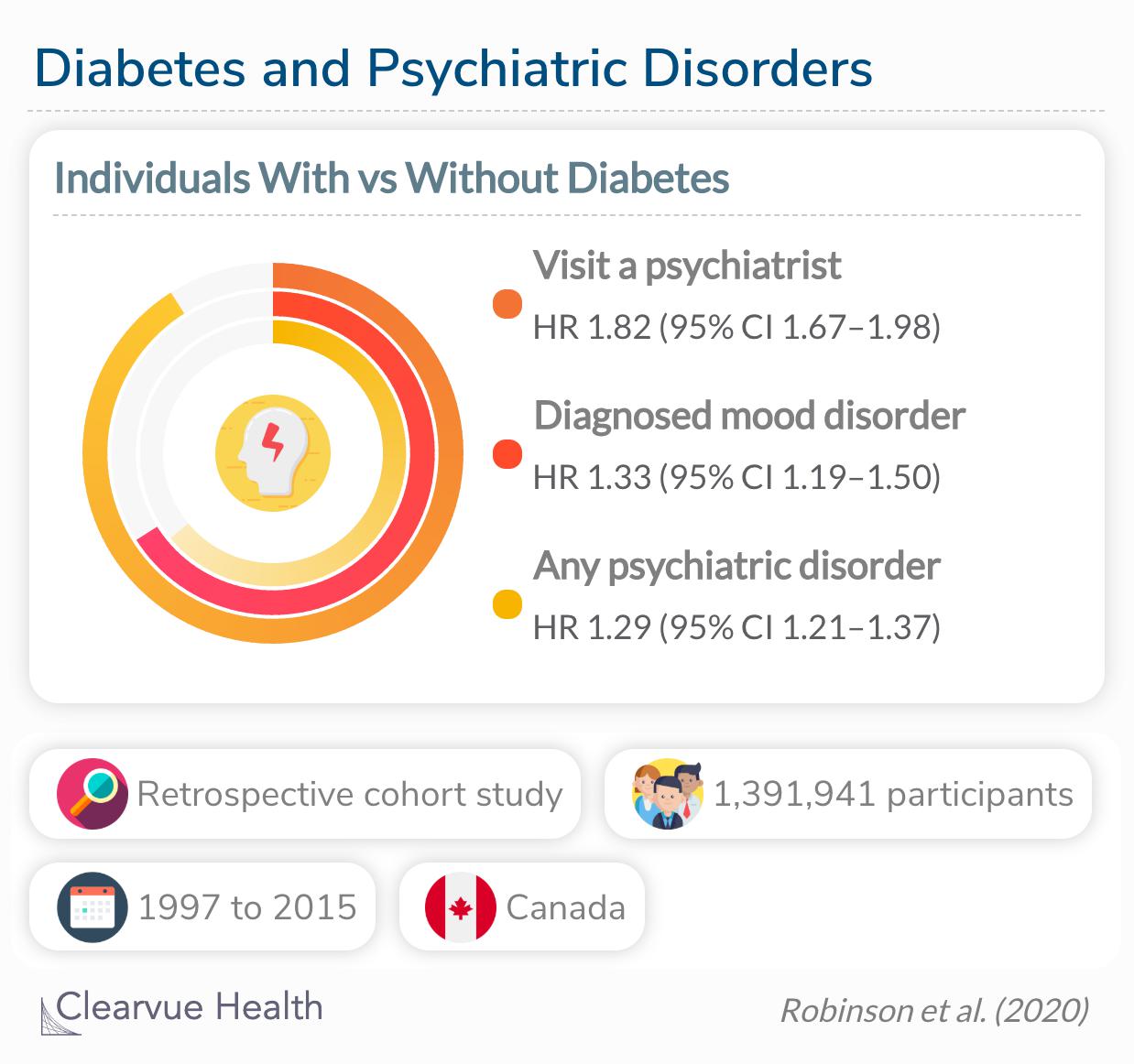
Diabetes and Psychiatric Disorders
A large study supported by the American Diabetes Association examined the psychiatric effect of diabetes on emerging adults (age 15-25) with type 1 diabetes. They analyzed a dataset from Canada that included the medical records of over a million adolescents.
Individuals with diabetes were more likely to suffer from a mood disorder (diagnosed in the emergency department or hospital) (adjusted hazard ratio 1.33 [95% CI 1.19–1.50]), visit a psychiatrist (1.82 [1.67–1.98]), and experience any type of psychiatric disorder (1.29 [1.21–1.37]) compared with their peers without diabetes.
Source: Risk of Psychiatric Disorders and Suicide Attempts in Emerging Adults With Diabetes
Within the dataset, the researchers pinpointed responses about psychiatric care. They found that participants with diabetes were more likely to have visited a psychiatrist and be diagnosed with a physiatric disorder over the study period compared to participants without diabetes. In particular, they found an even greater risk of mood disorders among participants with diabetes. This is strong evidence that diabetes status is a risk factor for psychiatric distress.
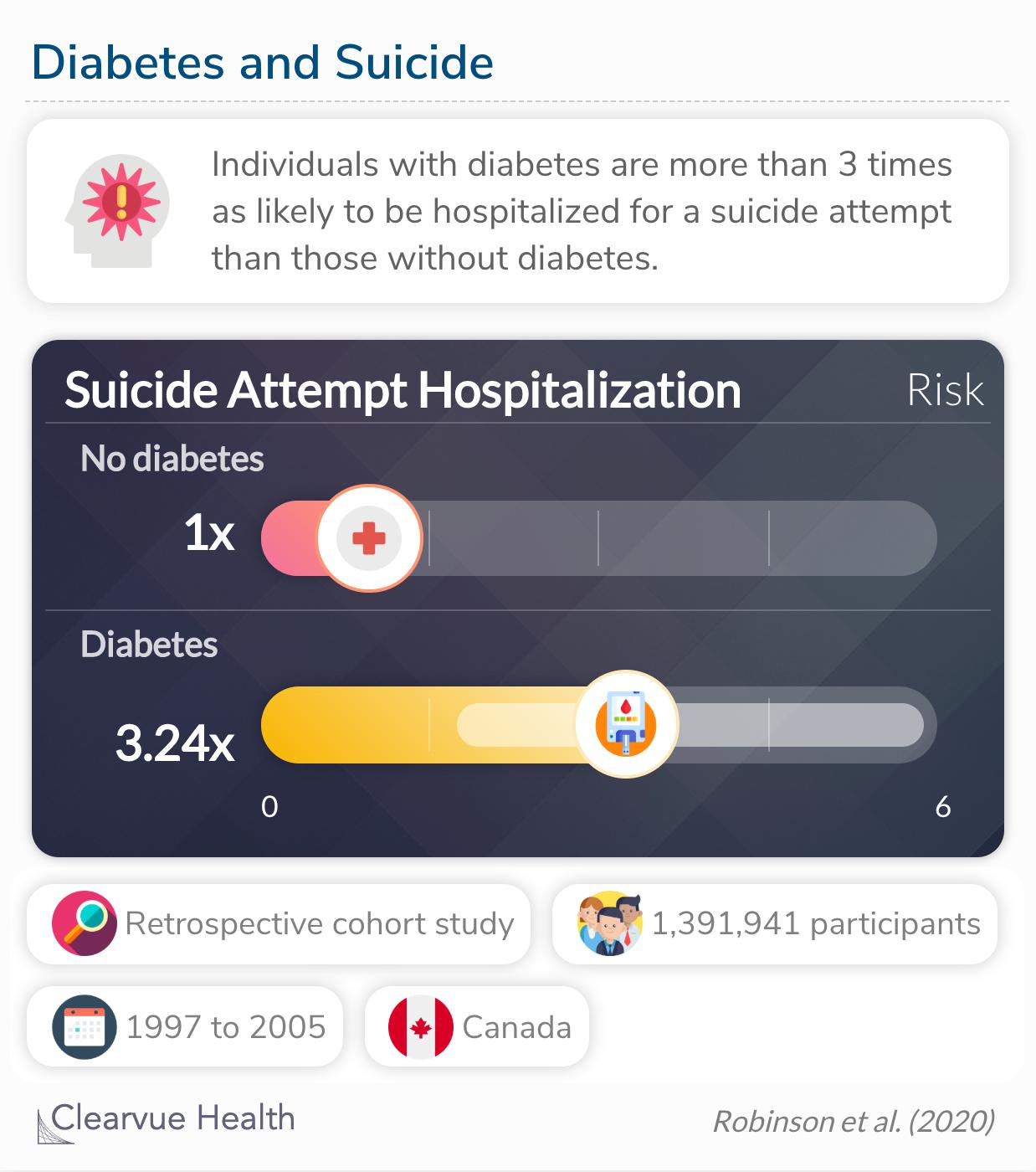
Diabetes and Suicide
The same study also examined suicide attempts. Suicide is a powerful indicator of psychiatric distress. They found that participants with type 1 diabetes were more than 3 times as likely to have been hospitalized for a suicide attempt compared to those without diabetes.
Individuals with (versus without) diabetes were more likely to be admitted to the hospital for a suicide attempt (3.24 [1.79–5.88]).
This statistic is alarming. However, we must also consider potential biases in the data. For example, the study only measured suicide attempts that resulted in hospitalization. This leaves out any suicide attempt that was not addressed by medical professionals. It also does not include suicidal ideation. We do not know the true number of suicide attempts or the true proportion of participants who considered suicide without this information.
In addition, there are many barriers to hospitalization. The likelihood of seeking medical treatment for a suicide attempt depends strongly on insurance status, living situation, age, transportation, social support, and many other factors. Measuring suicide by hospitalization may be biased against populations more impacted by these barriers.
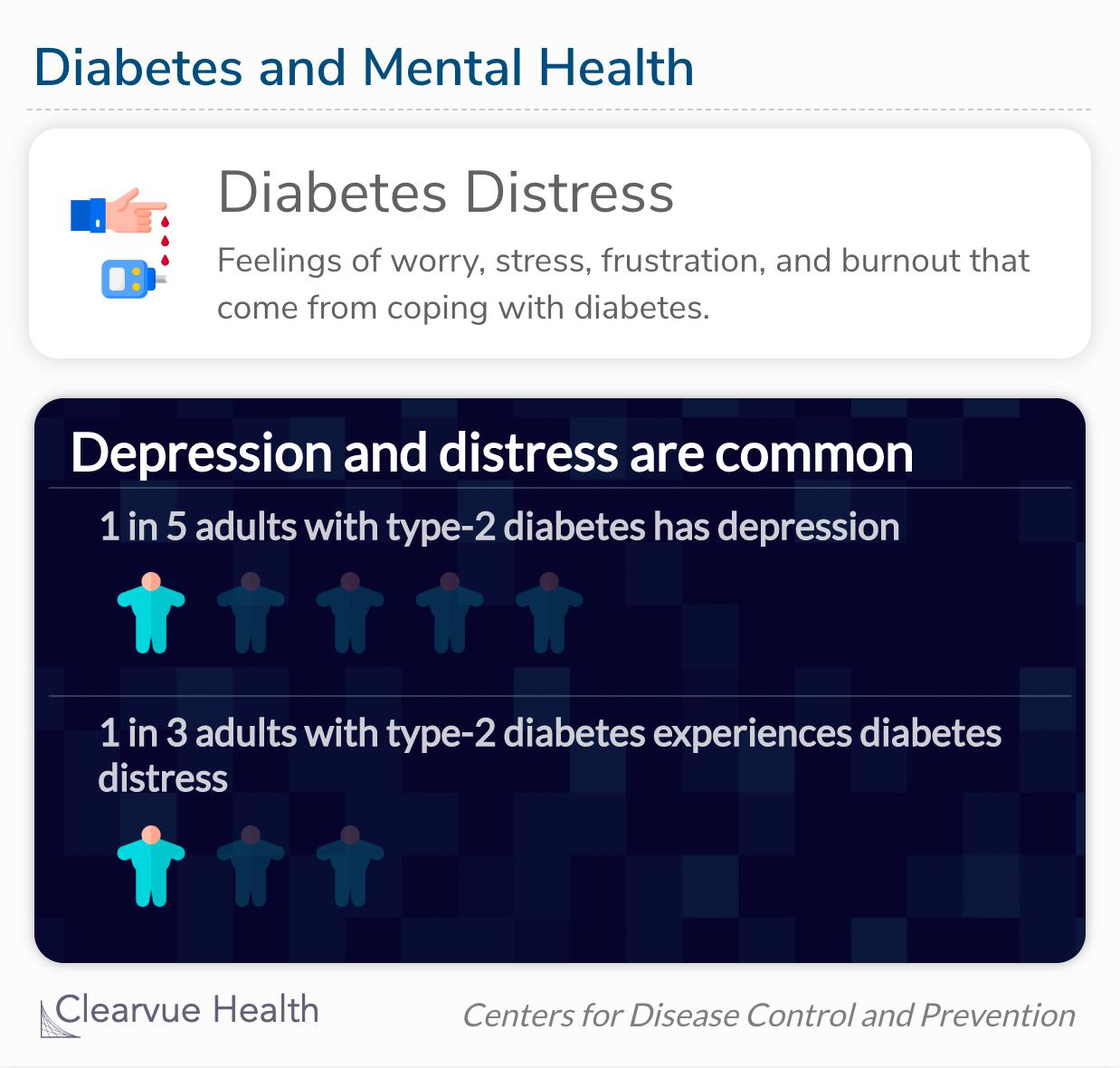
Diabetes Distress
The relationship between diabetes and mental distress is not a completely new concept. Diabetes distress has been used to describe the mental health struggles of those with diabetes. It can look like depression or anxiety, but it can not be treated effectively with medication. Treatment for diabetes distress must take diabetes-specific care into account.
Both depression and diabetes distress can increase the risk of serious health complications and early death.
Source: CDC Diabetes and Mental Health
Diabetes distress is a double-edged sword. Those who struggle with diabetes management are likely to feel distressed. Those who are distressed are likely to struggle with their diabetes care. In other words, diabetes can both cause distress and the distress can make it harder to take care of yourself. On top of that, stress hormones may to a physiological toll by impacting blood sugar levels.
Final thoughts
Young people with diabetes are more likely to visit a psychiatrist and be diagnosed with a psychiatric disorder. Studies have associated diabetes with increased rates of mood disorders and suicide attempts. People who feel overwhelmed may struggle to keep up with all the demands of diabetes management. Stress is known to impact sleep, diet, exercise, and attentiveness. This is why it is important to treat mental health as an integral part of diabetes care.