coronavirus and depression: how the pandemic has impacted depression rates
The coronavirus pandemic has caused pain to the world's population in a magnitude of ways. People are getting sick, their loved ones are dying, and healthcare workers are experiencing burnout like never before. Millions of people have lost their jobs, numerous companies filed for bankruptcy, and family-owned restaurants are permanently shutting down. Despair is everywhere. An undeniable number of people do not know how they will pay their rent and are on the brink of eviction. So when headlines about depression circle the newsrooms, it is not necessarily a shock to anyone. However, depression has been on the rise for years before coronavirus, and there are specific ways in which the pandemic has fueled the rise even further.
Risk factors for depression
According to the American Psychiatric Association, there are four key risk factors for depression: biochemistry, genetics, personality, and environment. As far as we know, the pandemic is not actively changing people's brain chemistry or genetic makeup. That leaves personality and environmental factors as the most impacted risk factors for depression in the pandemic.
Risk factors for depression include biochemistry in the brain, genetics, personality traits, and environmental factors.
Source: American Psychiatric Association
When a pandemic of this magnitude occurs, there is so much overload: graduations canceled, homeschooling, canceled vacations, not being able to hug your loved ones. Alone, each of these situations is stressful; together, they are overwhelming. In the meantime, violence and crime are still ever-present. Victims of child abuse and domestic abuse are trapped in quarantine with their abuser. Families in poverty have lost their jobs and their access to resources has been restricted due to office closures and no-contact rules. The list goes on, but you can see how each of these environmental circumstances are clear risk factors for depression.
Depression during the pandemic
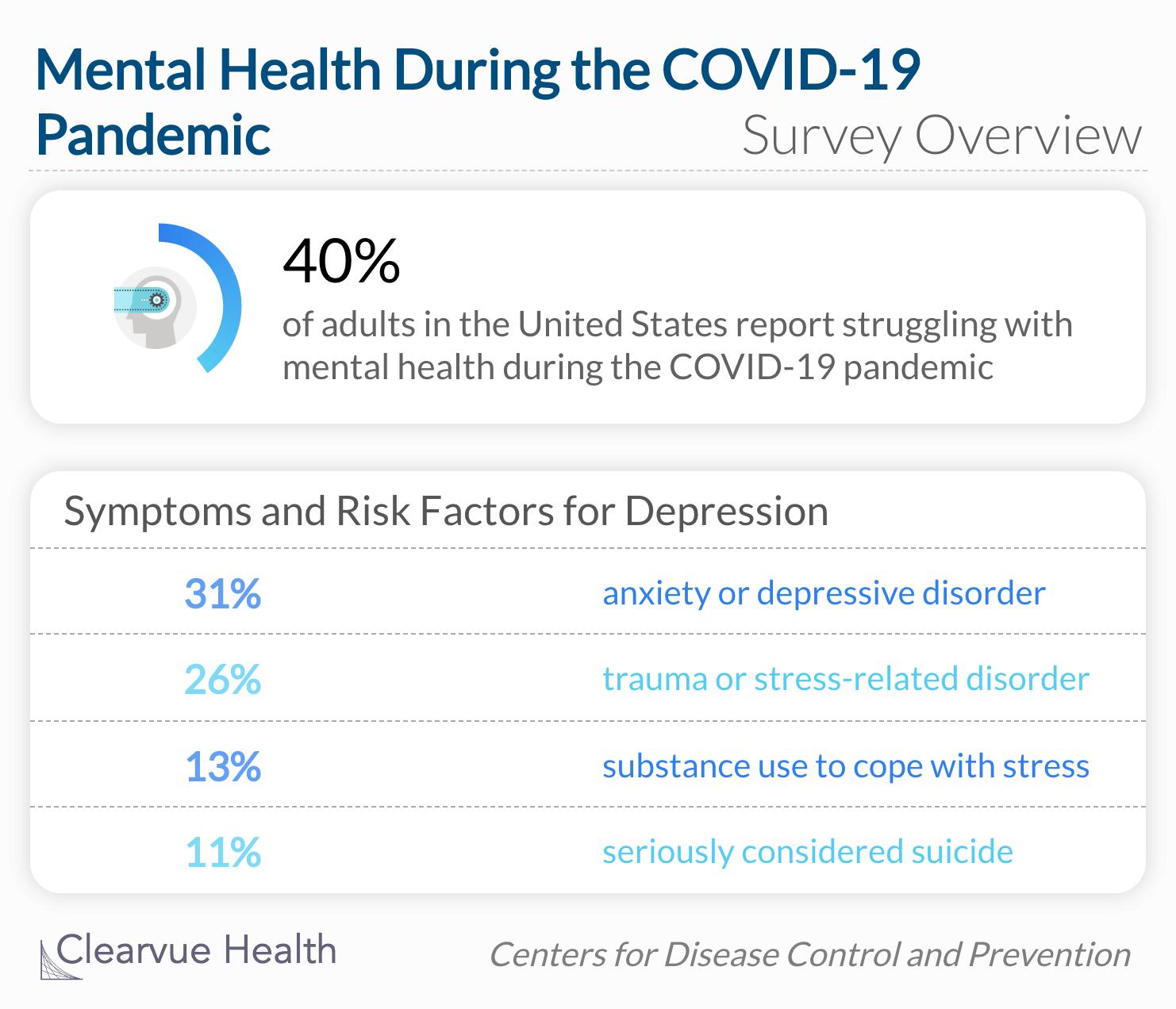
The Centers for Disease Control and Prevention released a survey between April and May of 2020 that measured the mental burden on participants since the start of the pandemic and subsequent lockdowns. Participants were asked about their medical history and current mental status. Survey questions also evaluated different types of mental health disorders and events.
Overall, 40.9% of 5,470 respondents who completed surveys during June reported an adverse mental or behavioral health condition, including those who reported symptoms of anxiety disorder or depressive disorder (30.9%), those with TSRD symptoms related to COVID-19 (26.3%), those who reported having started or increased substance use to cope with stress or emotions related to COVID-19 (13.3%), and those who reported having seriously considered suicide in the preceding 30 days (10.7%).
Source: Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020
A shocking 40% of adults reported struggling with mental health during the pandemic. A significant porportation of these adults reported anxiety and depressive disorders, as well as trauma or stress-related disorders. Concerningly, 13% of the sample said they turned to substance use as a means of coping with pandemic-induced stress, and 11% seriously considered suicide. These statistics are difficult to imagine and the mental healthcare system does not have the capacity to handle such a large number of cases.
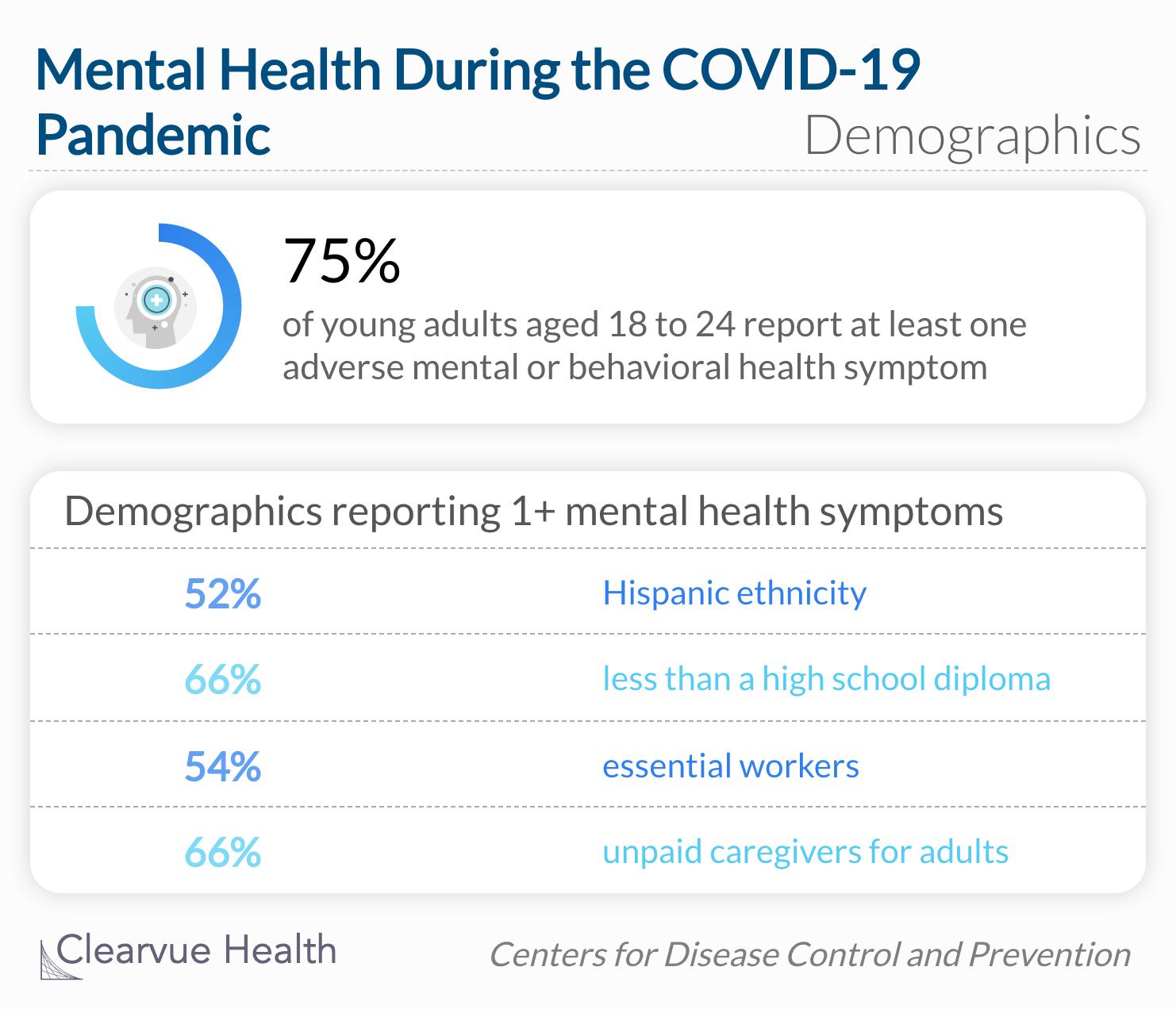
At least one adverse mental or behavioral health symptom was reported by more than one-half of respondents who were aged 18–24 years (74.9%) and 25–44 years (51.9%), of Hispanic ethnicity (52.1%), and who held less than a high school diploma (66.2%), as well as those who were essential workers (54.0%), unpaid caregivers for adults (66.6%), and who reported treatment for diagnosed anxiety (72.7%), depression (68.8%), or PTSD (88.0%) at the time of the survey.
Young adults between the ages of 18 and 24 had the highest percentage of adverse mental or behavioral health symptoms. This statistic is not incomprehensible when you really think about it. This age group is trying to graduate school, find a group of friends, apply for their first job, start a savings account, and all the other tasks associated with joining adulthood. Each of these endeavors is much harder to accomplish during the pandemic, if not impossible. However, the rise of mental health issues did not begin with the pandemic.
The preexisting rise of depression rates
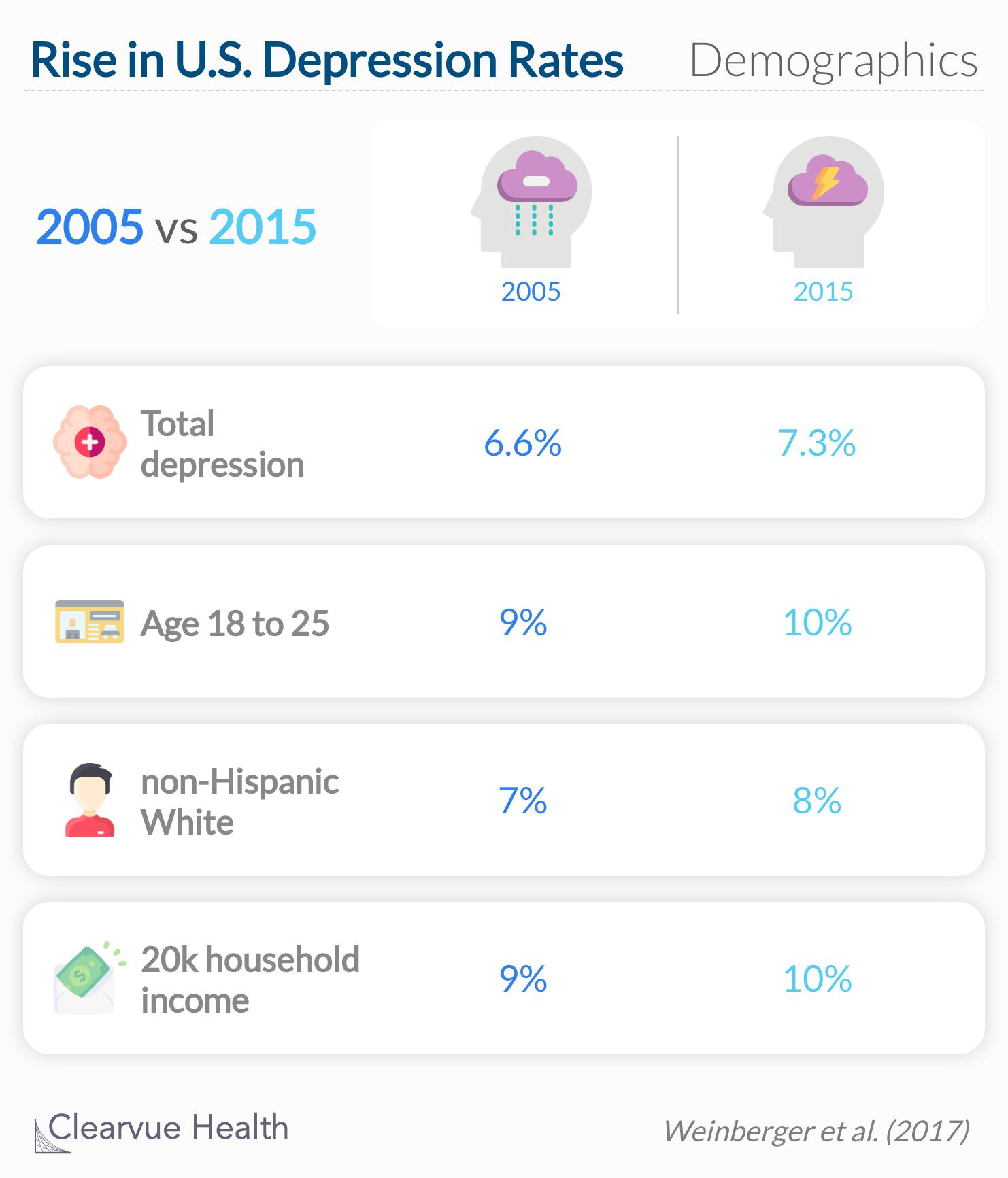
According to a study published in Psychological Medicine, the rate of depression in the United States was already on the rise before the pandemic. The study obtained data from the National Survey on Drug Use and Health and the US Census to compare depression rates in 2005 and 2015.
Depression prevalence increased significantly in the USA from 2005 to 2015, before and after controlling for demographics.
Source: Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups
According to this report, young, white, and low-income adults had significant increases in depression rates over the study period. The study also found that both men and women had an increase in depression rates, with men still reporting lower rates of depression than women. A 1% increase may seem small, but that is equivalent to roughly 3 million people in the United States. The statistical analysis also determined that these differences were significant, meaning that the two rates are distinctly different from one another.
Final thoughts
Assuming the survey respondents' answers represent the feelings of the general population, we can see that the pandemic has dramatically increased depression or at least negatively influenced people's perception of their mental health status. Psychologically validated risk factors for depression are targeted by the pandemic through the devastation of the infection and the drastic changes to societal norms. To help the population heal from this pandemic, we need more than just a vaccine. We need a strong mental healthcare system to support the well-being of those most affected.