Scleroderma
Evidence Based Answers
Scleroderma Diagnosis Overview
Scleroderma manifests through skin and organ involvement, observed in clinical evaluations. Diagnosis is supported by serologic markers, like ANA tests. Early symptom detection is key for effective management.
Scleroderma impacts skin and organs, needing serologic tests and early detection.
Beyond Skin Changes: Exploring Scleroderma Symptoms
Scleroderma is primarily known for causing hard, thick skin. However, it can also affect various organs, leading to issues like lung fibrosis, kidney problems, and heart complications.
In addition to skin changes, patients might feel joint pain, stiffness, and swelling that can interfere with daily activities. Comprehensive evaluation by a healthcare provider is necessary to identify the condition accurately.
In addition to skin changes, patients might feel joint pain, stiffness, and swelling that can interfere with daily activities. Comprehensive evaluation by a healthcare provider is necessary to identify the condition accurately.
“
Source Quotes:
Skin involvement is a nearly universal feature of SSc.,Patients with dсSЅc are more likely to have a rapid progression of skin thickening with early development of lung fibrosis and an increased risk of renal crisis and cardiac involvement.
Understanding Laboratory Tests for Scleroderma
Diagnosing scleroderma often involves specific blood tests called serologic markers. One of these tests is the antinuclear antibody (ANA), which is positive in about 95% of patients with scleroderma. However, due to varying sensitivity, multiple tests might be needed to confirm the diagnosis.
Interpreting these test results can be challenging as they are typically combined with clinical observations to make an informed diagnosis.
Interpreting these test results can be challenging as they are typically combined with clinical observations to make an informed diagnosis.
“
Source Quotes:
Positive anti-topoisomerase I (anti-Scl-70) antibody, anticentromere antibody (ACA), and/or anti-RNA polymerase III antibody; or a positive antinuclear antibody (ANA) with a nucleolar immunofluorescence pattern.,Antinuclear antibody (ΑΝA). ANΑ test is positive in approximately 95 percent of patients with SSc, and therefore a negative test should prompt consideration of other fibrosing illnesses.
Clinical Signs and Evaluation in Scleroderma
When systemic sclerosis, a type of scleroderma, is suspected, initial evaluations focus on symptoms like unusual skin thickening, Raynaud's phenomenon, and swollen fingers.
Alongside examining these clinical signs, specific serological markers are assessed to confirm the presence and type of scleroderma.
Alongside examining these clinical signs, specific serological markers are assessed to confirm the presence and type of scleroderma.
“
Source Quotes:
Systemic sclerosis (SSc) should be suspected in patients presenting with Raynaud Phenomenon (RP), skin thickening, puffy or swollen fingers, hand stiffness, and painful distal finger ulcers.,Early referral to specialists, depending upon the pattern of organ involvement and severity of disease, is often appropriate.
Pulmonary Challenges in Scleroderma
Pulmonary issues are common in scleroderma, affecting more than 80% of patients. The key problems include lung scarring, known as fibrosis, and high blood pressure in the lung's arteries, termed pulmonary hypertension.
Identifying lung involvement can manage symptoms like breathlessness and a persistent dry cough, which can help prevent severe complications.
Identifying lung involvement can manage symptoms like breathlessness and a persistent dry cough, which can help prevent severe complications.
“
Source Quotes:
Some degree of pulmonary involvement is present in more than 80 percent of patients with SSc.,The two principal clinical manifestations are ILD (also called fibrosing alveolitis or pulmonary fibrosis) and pulmonary vascular disease, leading to pulmonary arterial hypertension.
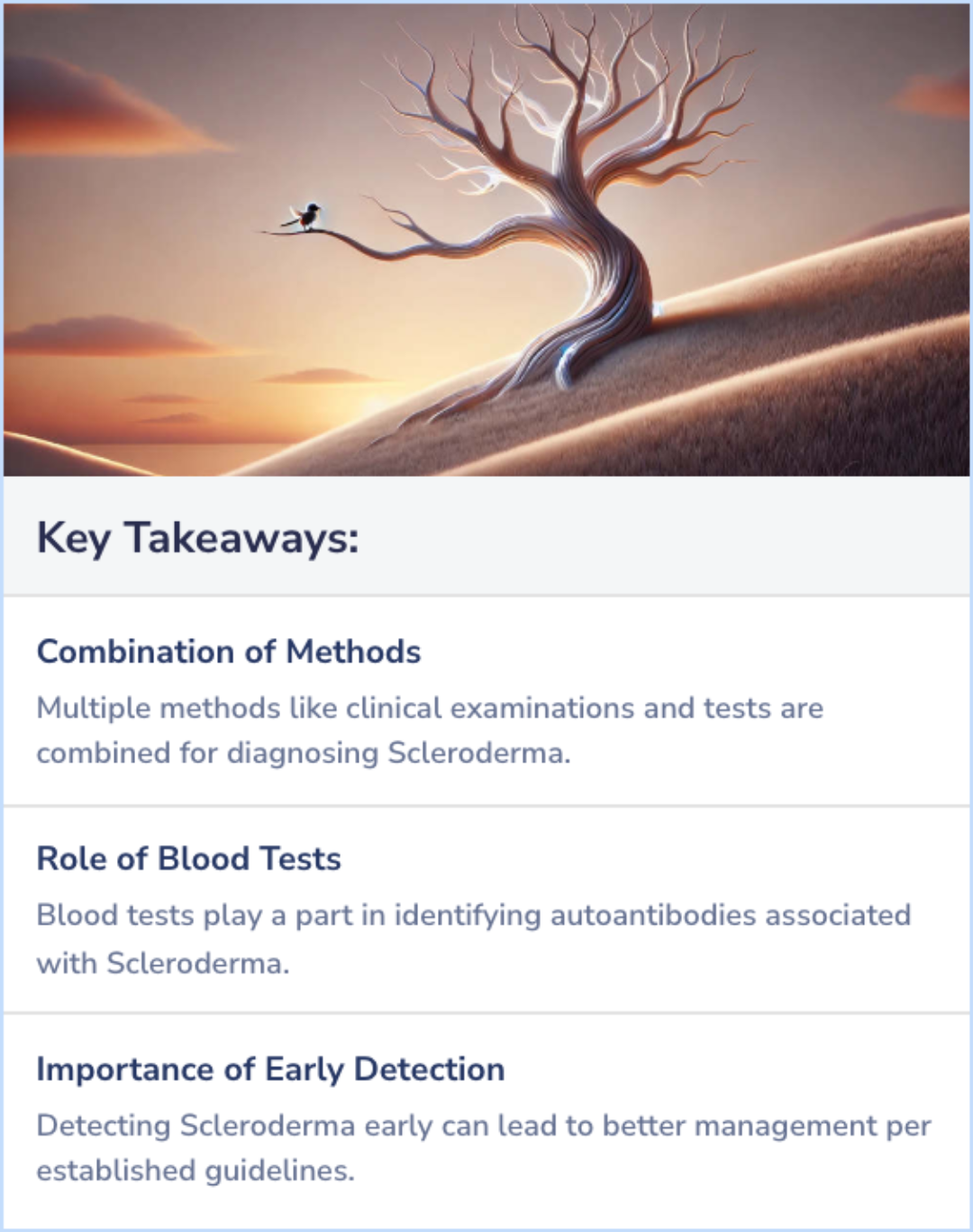
Key Takeaways
Conclusions
Scleroderma, a complex autoimmune disorder, is diagnosed through a combination of clinical examination and specific tests. These tests can include blood tests to check for autoantibodies and imaging tests to assess internal organ involvement.
Studies emphasize that early detection and diagnosis can qualify individuals for more effective management, which is supported by established guidelines that direct healthcare professionals.
Studies emphasize that early detection and diagnosis can qualify individuals for more effective management, which is supported by established guidelines that direct healthcare professionals.
Literature Review
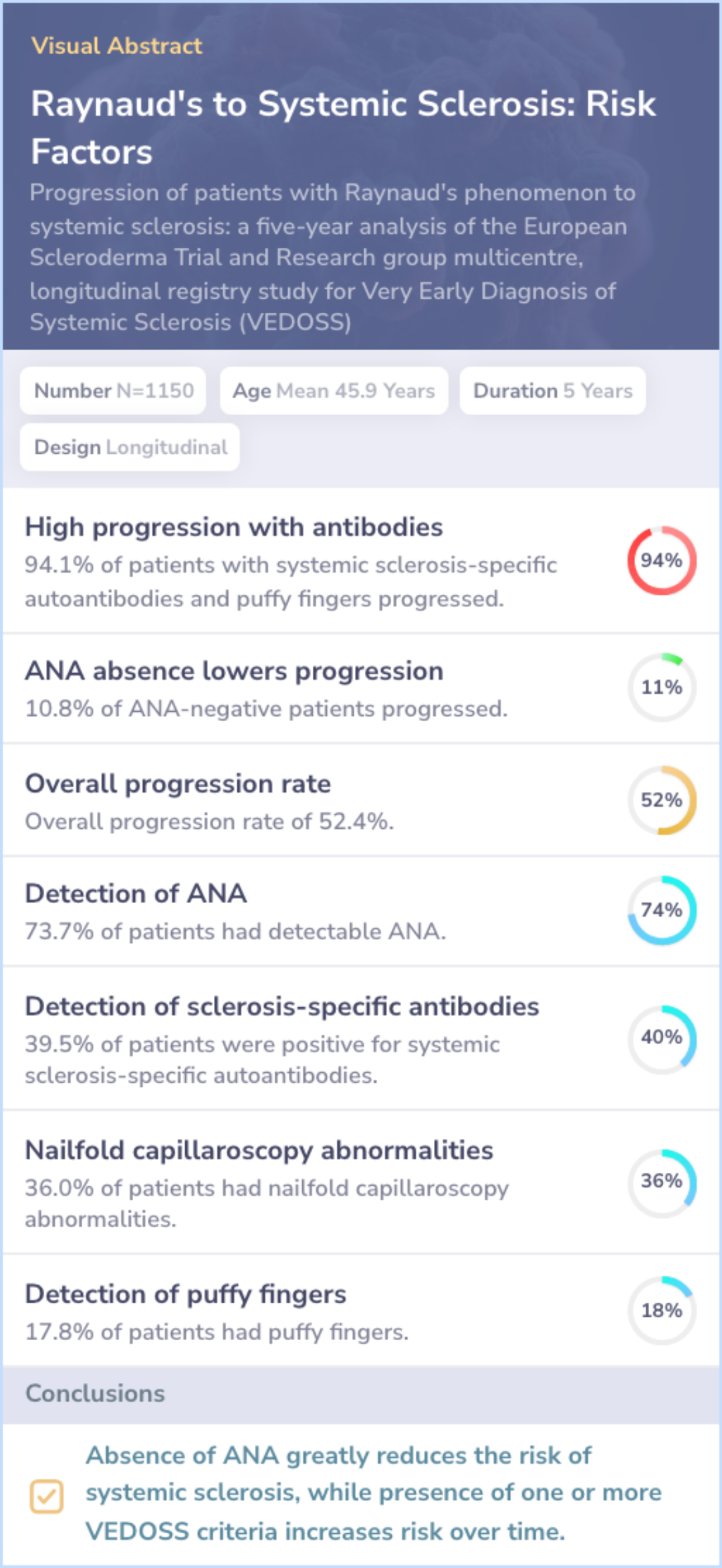
Bellando-Randone, 2021
Study Overview:
Study aims to assess VEDOSS criteria: Focuses on predicting systemic sclerosis in patients with Raynaud's phenomenon.
Inclusion and exclusion criteria: Patients with Raynaud's and without established systemic sclerosis at enrolment were included.
Findings:
Progression metrics: 52.4% progression rate to systemic sclerosis in study period.
ANA as a protective factor: ANA negativity strongly linked to lower risk of progression.
Interpretation:The study provides a risk stratification tool using VEDOSS criteria for managing Raynaud's patients and guiding early intervention.
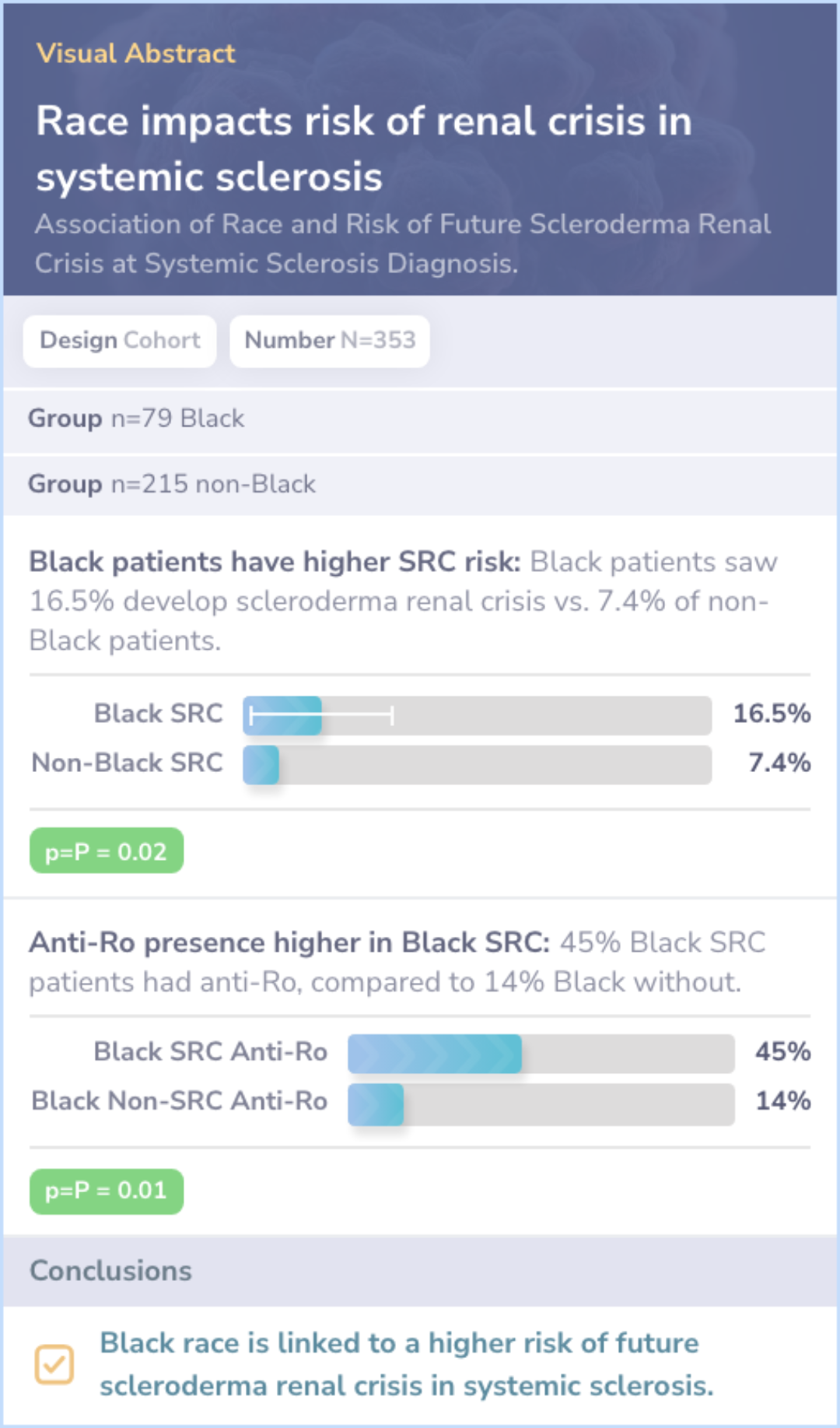
Literature Review
Forman, 2023
Study Objective:Investigates racial differences in the development of scleroderma renal crisis within systemic sclerosis patients.
Key Findings:
Black Patients: Higher risk of developing scleroderma renal crisis, 16.5% compared to 7.4% in non-Black patients.
Adjustments: Risk assessment adjusted for age, kidney function, hypertension, and protein in urine.
Antibody Associations: Anti-Ro antibody linked with higher rates in Black patients with the crisis.