Psoriasis
Evidence Based Answers
Psoriasis Pathogenesis Overview
Psoriasis involves the immune system and pathways like IL-23/Th17, driven by dendritic cells and genetic factors. These elements contribute to inflammation and skin growth, with therapies targeting these pathways to manage the disease effectively.
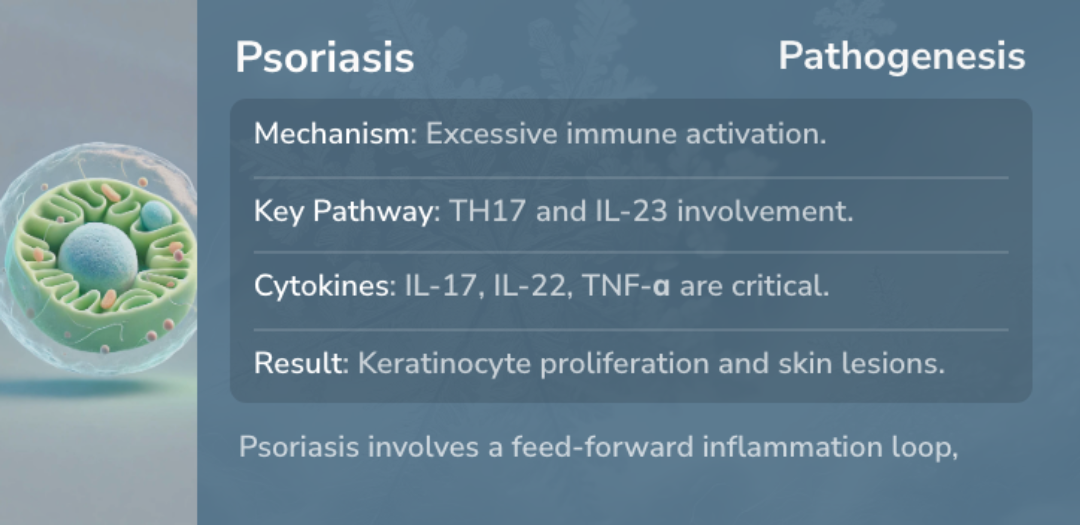
Immune cells and pathways drive psoriasis, highlighted by IL-23/Th17 activity and dendritic cell roles.
Psoriasis and the Immune System
Psoriasis is a chronic disease driven by the immune system, involving T lymphocytes, dendritic cells, and cytokines like IL-23, IL-17, and TNF. These immune components trigger inflammation and lead to abnormal skin cell growth.
The understanding of the immune system's role has revolutionized treatment options. Biologic therapies target specific immune pathways, offering more effective solutions for managing chronic plaque psoriasis.
The understanding of the immune system's role has revolutionized treatment options. Biologic therapies target specific immune pathways, offering more effective solutions for managing chronic plaque psoriasis.
“
Source Quotes:
Psoriasis is a complex immune-mediated disease in which T lymphocytes, dendritic cells, and cytokines (interleukin [IL] 23, IL-17, and tumor necrosis factor [TNF]) play a central role.
Disturbances in the innate and adaptive cutaneous immune responses are responsible for the development and sustainment of psoriatic inflammation.
The IL-23/Th17 Pathway in Psoriasis
The IL-23/Th17 pathway is crucial in psoriasis pathogenesis, promoting both inflammation and excessive skin cell growth. IL-23 activates Th17 cells, which release proinflammatory cytokines like IL-17, perpetuating the cycle of inflammation.
New therapies targeting this pathway have emerged, significantly reducing disease severity for many patients.
New therapies targeting this pathway have emerged, significantly reducing disease severity for many patients.
“
Source Quotes:
The IL-23/Th17 axis is the central driver of immune activation, chronic inflammation and keratinocyte proliferation.
The TNFα–IL-23–Th17 inflammatory pathway characterizes plaque-type psoriasis.
Dendritic Cells and Psoriasis
Dendritic cells play a key role in triggering and sustaining psoriatic inflammation. These cells activate T cells and support the production of cytokines like TNF-alpha and IL-1-beta, maintaining a chronic inflammatory state.
Their contribution to the disease highlights the importance of therapies that modulate dendritic cell activity.
Their contribution to the disease highlights the importance of therapies that modulate dendritic cell activity.
“
Source Quotes:
It is well known that dendritic cells play a major role in the initial stages of disease.
Activation of myeloid dendritic cells by tumor necrosis factor (TNF)-alpha, interferon-gamma, interleukin (IL) 6, and IL-1-beta stimulates the adaptive immune system via IL-23.
Genetics and Psoriasis
Psoriasis has a strong genetic component, with over 60 genetic markers linked to the disease. These genes interact with immune pathways, influencing how the disease develops and progresses.
Research into these genetic factors provides insight into the complex interactions between genes and immune triggers, opening doors to more precise therapies.
Research into these genetic factors provides insight into the complex interactions between genes and immune triggers, opening doors to more precise therapies.
“
Source Quotes:
More than 60 susceptibility loci have now been identified using genome-wide association studies.
Psoriasis has a genetic component that is supported by patterns of familial aggregation.
Key Takeaways
Conclusions
Psoriasis is fundamentally driven by immune system interactions, notably involving T lymphocytes, dendritic cells, and cytokines like IL-23, IL-17, and TNF, which trigger inflammation and abnormal skin cell growth.
The IL-23/Th17 pathway is central to both inflammation and cell growth, with new therapies targeting this pathway showing reductions in disease severity. Dendritic cells further sustain inflammation by activating T cells and cytokines.
Genetic factors, with over 60 linked markers, are also influential, interacting with immune pathways and offering insights into precise therapeutic options.
The IL-23/Th17 pathway is central to both inflammation and cell growth, with new therapies targeting this pathway showing reductions in disease severity. Dendritic cells further sustain inflammation by activating T cells and cytokines.
Genetic factors, with over 60 linked markers, are also influential, interacting with immune pathways and offering insights into precise therapeutic options.
Literature Review
Schwarz
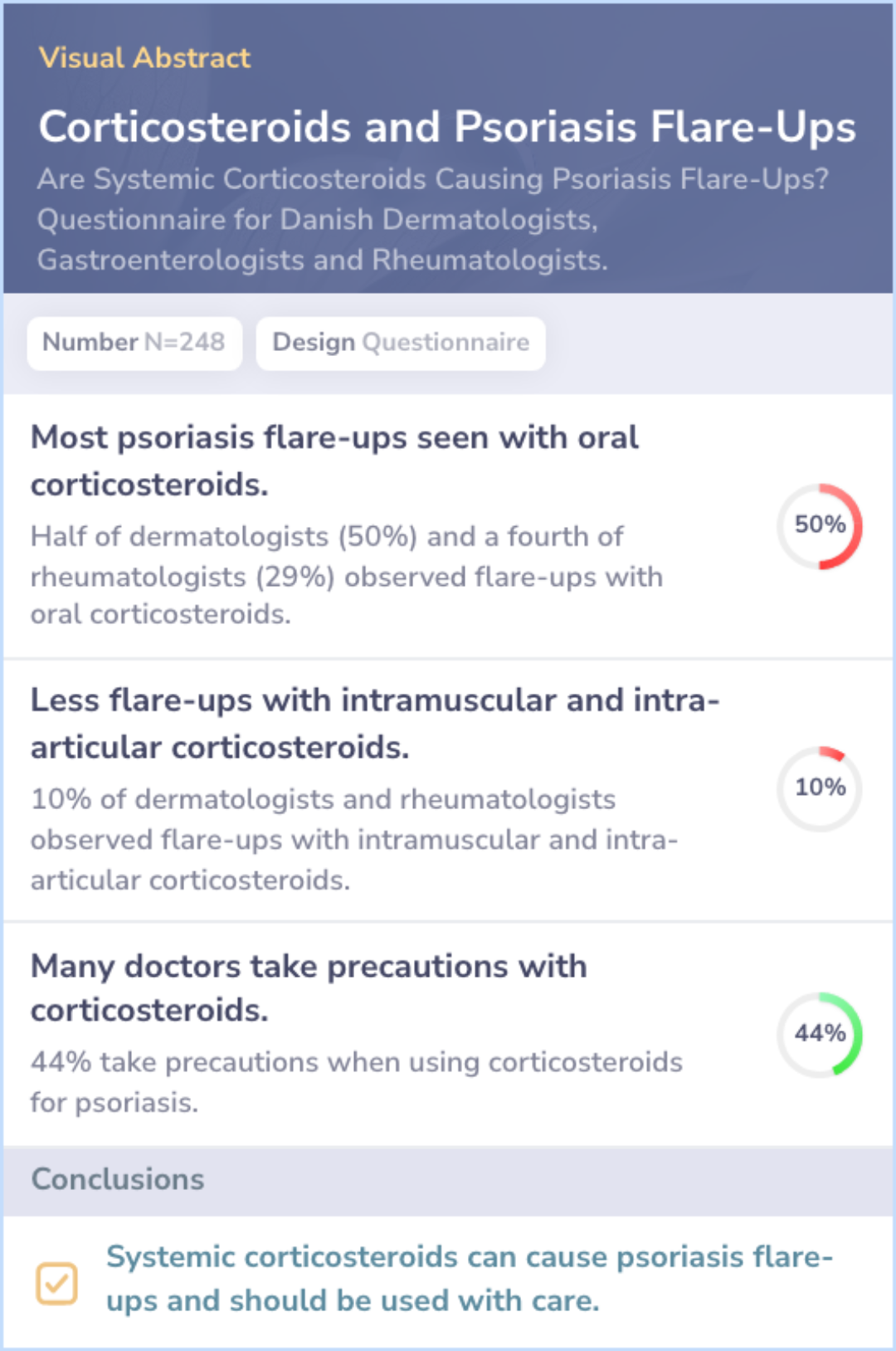
Physician Observations:
Psoriasis flare-ups linked to treatments: 50% of dermatologists and 29% of rheumatologists observed flare-ups after oral corticosteroids.
Less frequent with other corticosteroids: 10% of both groups observed flare-ups with intramuscular or intra-articular corticosteroids.
Precautions during treatment: 44% of respondents reported taking precautions with corticosteroid treatments.
Treatment Preferences:Intra-articular corticosteroids were most used, exclusively by rheumatologists.
Study Conclusion:Corticosteroids can cause psoriasis flare-ups and should be used cautiously.
Literature Review
Liu Z
Role of Immunosenescence in Psoriasis:
Immunosenescence defined: Aging-related immune dysfunction and inflammation are linked.
Inflammaging in detail: Chronic inflammation with high pro-inflammatory markers.
Impact on T-cells: Premature T-cell senescence and altered immune cell ratios.
Literature Review
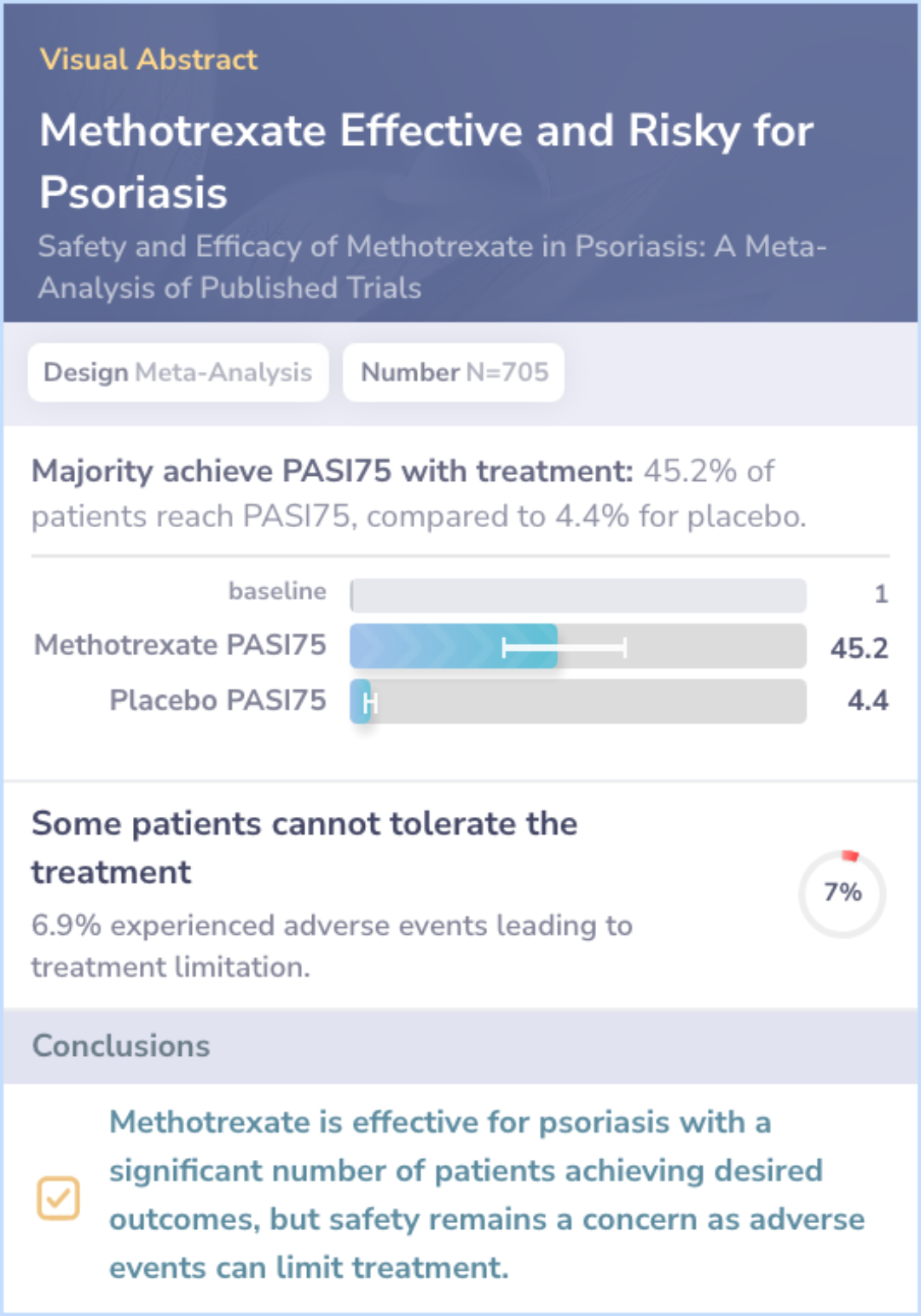
West, 2023
Efficacy of Methotrexate:
Patient response: 45.2% of patients achieved significant improvement.
Comparison with placebo: PASI75 for placebo calculated at 4.4%.
Safety Outcomes:
Adverse events: Treatment limiting in 6.9% of patients over six months.
Safety data sources: Included studies from other conditions like rheumatoid arthritis.