MCTD
Evidence Based Answers
MCTD Treatment Strategies
MCTD treatment includes calcium blockers for Raynaud's, immunosuppressants for lung issues, and new drugs like selexipag for pulmonary hypertension. There's ongoing research for tailored approaches.
Calcium channel blockers aid Raynaud's, immunosuppressants target lung issues, and selexipag advances PH treatment.
Managing Raynaud's Phenomenon in MCTD
Raynaud's Phenomenon (RP) is often seen in Mixed Connective Tissue Disease (MCTD). This condition reduces blood flow to areas like fingers and toes, making them pale or blue. Symptomatic relief is usually through staying warm and avoiding smoking and caffeine.
For RP, calcium channel blockers, such as nifedipine, help increase blood flow by affecting blood vessels and heart muscles. Severe cases might be treated with intravenous prostaglandins like iloprost.
For RP, calcium channel blockers, such as nifedipine, help increase blood flow by affecting blood vessels and heart muscles. Severe cases might be treated with intravenous prostaglandins like iloprost.
“
Source Quotes:
Symptomatic treatment of RP, the most common symptom of MCTD, consists of general advice (keeping warm, and avoiding injury, smoking, and caffeine).,Treatment with oral calcium channel blockers that block voltage-gated calcium channels (VGCCs) in cardiac muscle and blood vessels decreases total peripheral resistance and increases the peripheral blood flow with effects on RP.
Immunosuppressive Therapies for MCTD
MCTD often causes inflammation, which can be managed with corticosteroids such as prednisone. These medications help when conditions like fever, arthritis, and rashes are present. However, not all symptoms respond the same way, and some might need stronger treatments like cyclophosphamide.
For lung-related issues linked with MCTD, different immunosuppressants are used based on the condition's complexity.
For lung-related issues linked with MCTD, different immunosuppressants are used based on the condition's complexity.
“
Source Quotes:
Patients diagnosed of MCTD were initially described as having a good prognosis, being extremely responsive to corticosteroid therapy.,Corticosteroids (prednisone and methylprednisolone) and cytotoxic agents, most often cyclophosphamide, are the most frequently employed immunosuppressants.
Approaches to Pulmonary Hypertension in MCTD
Pulmonary Hypertension (PH) is a possible complication of MCTD. Treatments are often adapted from methods for other types of PH, such as those seen in systemic sclerosis. This includes using endothelin receptor antagonists and phosphodiesterase 5 inhibitors along with traditional vasodilators if effective.
Selexipag, an oral medication, has shown potential in treatment-resistant cases, indicating advancements in managing this condition.
Selexipag, an oral medication, has shown potential in treatment-resistant cases, indicating advancements in managing this condition.
“
Source Quotes:
PAH can be more specifically treated with endothelin receptor antagonists (bosentan, ambrisentan, or macitentan), phosphodiesterase 5 inhibitors (sildenafil, tadalafil, or vardenafil), and prostanoids (epoprostenol, treprostinil, or inhaled iloprost).,Recent reports indicate that selexipag, an oral, selective prostacyclin receptor, shows promise.
Immunosuppression is indicated only in select cases of pulmonary arterial hypertension related to CTD; more commonly, selective pulmonary vasodilators are used.
Management of Interstitial Lung Disease in MCTD
Interstitial Lung Disease (ILD) is common in MCTD, needing specific approaches. Detection uses tools like echocardiography and CT scans. In mild cases, regular monitoring is suggested, and treatments may include certain drugs like calcium channel blockers and immunosuppressants.
Antifibrotic drugs like nintedanib or pirfenidone can help slow disease progression in advanced cases. Lung transplant might be considered for severe, non-responsive scenarios.
Antifibrotic drugs like nintedanib or pirfenidone can help slow disease progression in advanced cases. Lung transplant might be considered for severe, non-responsive scenarios.
“
Source Quotes:
Lung involvement is common in patients with MCTD, varying from 47% to 78%.,Immunosuppression is the mainstay of treatment for ILD, although data from randomized controlled trials (RCTs) to support specific treatments are lacking.
Antifibrotic therapy with nintedanib or pirfenidone slows annual FVC decline by approximately 44% to 57% in individuals with IPF, scleroderma associated ILD, and in those with progressive pulmonary fibrosis of any cause.
Key Takeaways
Conclusions
Recent studies highlight various approaches for managing Mixed Connective Tissue Disease (MCTD), focusing on symptom management and improving patient quality of life. Research underscores the importance of utilizing a combination of medications and lifestyle modifications, guided by clinical guidelines.
Tailored strategies are recommended, with ongoing evaluation and adaptation to individual patient responses being a consistent theme in MCTD treatment plans.
Tailored strategies are recommended, with ongoing evaluation and adaptation to individual patient responses being a consistent theme in MCTD treatment plans.
Literature Review
Jovancevic, 2013
Study Purpose:Investigated effects of anti-B cell treatment in mixed connective-tissue disease with autoimmune thrombocytopenia resistant to standard treatments.
Treatment Process:
Rituximab Use: Used on 16 female patients, given intravenously over four weeks.
Patient Demographics: Patients had median age of 36 and included three with mixed connective-tissue disease.
Results:
B Cell Depletion: Achieved in 94% of cases one month after treatment.
Platelet Counts: Significant increase observed within one month.
Treatment Efficacy:Overall response rate was 80% according to literature review of similar cases.

Literature Review
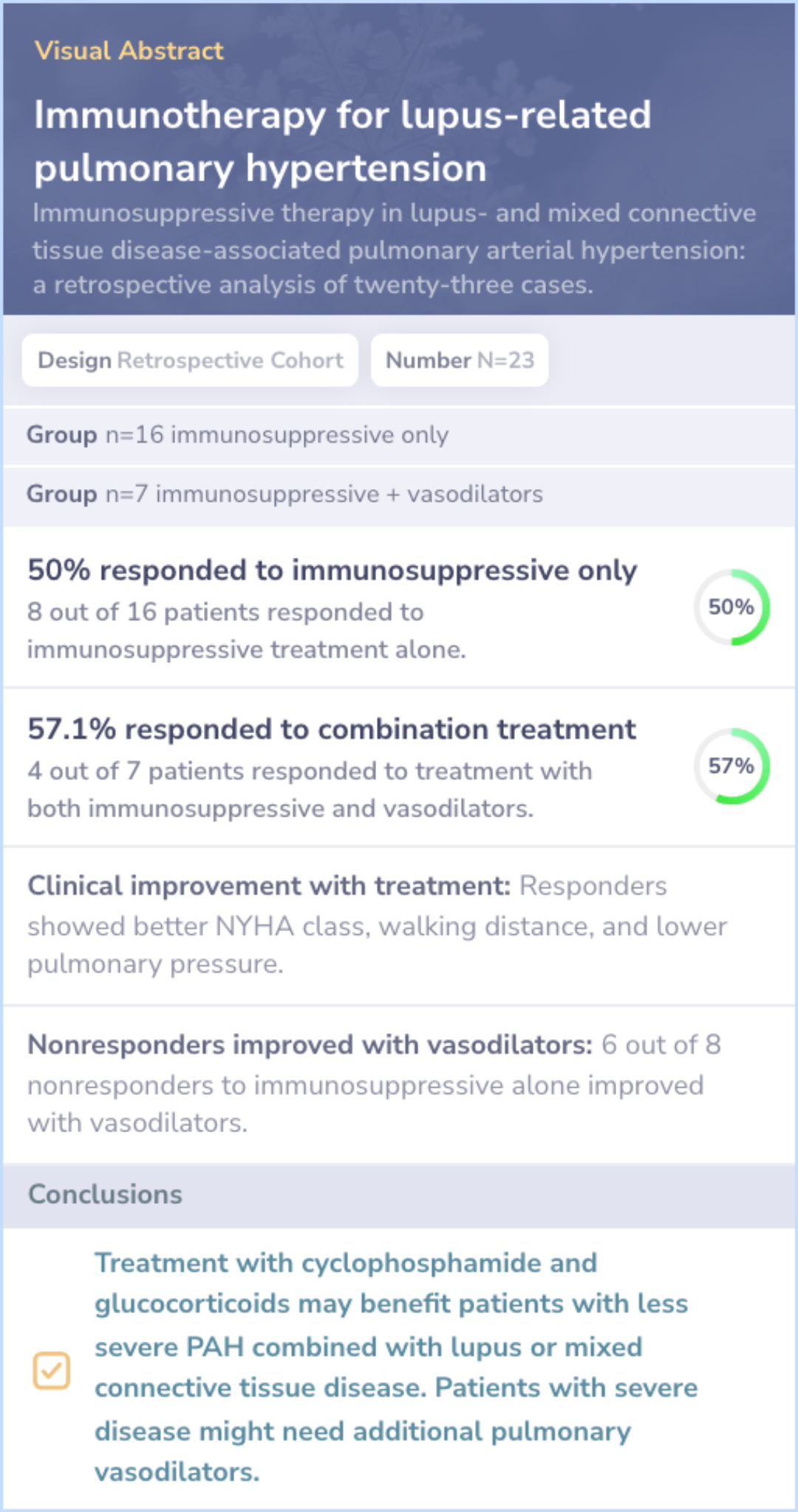
Jais, 2008
Main Finding:Immunosuppressive therapy alone resulted in a positive response in 50% of patients with MCTD-related PAH.
Variable Response:
Less severe cases benefit more: Patients with less severe symptoms showed better response to treatment.
Combination therapy: Pulmonary vasodilators benefited 6 of 8 nonresponders to immunosuppressive therapy.
Response monitoring: Clinical and hemodynamic criteria are important for monitoring treatment response.